
Caregiving: A bittersweet journey
A look at life before and after becoming a caregiver.
“For Lalita, each day grew more difficult than the previous one. She felt as though she needed to be everywhere at once — along with being there for her nephew Abhinav, who had a congenital heart disease, she was taking care of the household chores, preparing food for everyone, spending time with her son, and tending to her mother-in-law, who was suffering from diabetes-related complications. She felt exhausted always and would feel excruciating pain in her body at the end of each day. Her nights were filled with anxiety and she seldom had a good night’s sleep.”
Family caregivers like Lalita are at the heart of Noora Health’s Care Companion Program (CCP), which equips them with essential life-saving skills to better care for their loved ones. From the moment a health issue arises, caregivers step in to provide physical, emotional, and financial support, ensuring the well-being and comfort of those in their care.
Being a caregiver is both rewarding and difficult, demanding time, energy, and patience — frequently disrupting the caregiver’s life and well-being. In order to create a more holistic support system for caregivers, it is vital for us at Noora Health to understand the challenges caregivers face in depth.
In 2023, The Caregiving Lab undertook a design research initiative aimed at exploring the experiences, challenges, and support available to caregivers of people with high-risk, life-threatening conditions. These included cancer, heart diseases, life-altering accidents, congenital conditions, and other areas that require intensive treatment and long-term care.
Over the course of six months, we conducted in-depth interviews and group sessions with 19 extreme users, across urban and rural Karnataka, in India. This helped us understand what their lives looked like before becoming caregivers, and how it changed once they took on the role.
The nine burdens of a caregiver
Through our research, we identified nine interrelated areas where caregivers felt their lives had changed dramatically, post embarking on their caregiving journey.
1. Housework
“I didn’t trust anyone with food hygiene. I preferred to wash all the vegetables myself to ensure they were extra clean.” — A caregiver whose infant son has a hole in his heart and a hernia
Our research reaffirmed the fact that women and their older daughters often became caregivers by default. Before becoming a caregiver, regular household responsibilities included general cleaning, grocery shopping, and managing laundry. However, as a caregiver, these responsibilities expanded to include extra precautions such as sanitizing the house to prevent infections for the patient and separating out space for the patient which otherwise may be shared. This increased workload often resulted in limited time available for general house upkeep and management, and added to caregivers’ burden of household responsibilities, especially among women.
2. Food and nutrition
“He angrily asked me why he couldn’t eat the same food as me.” — A caregiver of an 8-year-old child with a congenital heart condition
Accentuating the gendered nature of domestic work, women often defaulted to household cooking responsibilities and preparing family meals.
As caregivers, they additionally had to prepare an extra meal tailored to the patient’s dietary restrictions.
More often than not, they were also the ones who fed the patient. Considering most families have three to five meals a day, becoming a caregiver meant additional food-related responsibilities and took up a significant amount of their time daily.
In some instances, caregivers shared how the family’s usual diet had to be changed to accommodate the needs of the patient. This was either because it was easier to cook one common meal for all family members, or an act of solidarity from the family to support the patient with restrictions. Sometimes, it was also due to increasing financial stress and the unaffordability of certain food items, with the more expensive foods being reserved for the patient.
3. Hygiene-related tasks
“She is very heavy and it is difficult for me to lift her alone. I also can’t ask my brother to help with tasks like bathing her and taking her to the washroom.” — A caregiver whose mother has advanced diabetes and gangrene
Upon assuming the role of a caregiver, people often found themselves responsible for the patient’s personal hygiene, including tasks such as assisting with baths and accompanying them to the washroom. Often this involved lifting of patients and was impossible for women caregivers to take on alone, especially when the patient weighed significantly more than them or experienced some form of paralysis. As a result, this was one category of caregiver duties where we saw men chip in due to their muscular strength.
Supporting hygiene-related tasks also created some discomfort between both patients and caregivers, especially when they were of different genders.
4. Healthcare interactions
“I don’t like injections, they make me faint. Giving them to another person was very difficult for me.” — A caregiver whose mother-in-law had a stroke
The caregiver’s role is multifaceted, encompassing a spectrum of tasks related to the patient’s medical care. This includes overseeing the diagnostic process, coordinating treatments and interventions, managing follow-ups, ensuring timely medicine refills, organizing necessary tests, and addressing personal healthcare needs. Additionally, caregivers may also take on critical responsibilities such as administering injections, dressing wounds, and overseeing medication adherence. As a result, caregivers often neglected their own physical and mental health in an effort to be continuously available for the patient. When their own issues became overwhelming, caregivers resorted to short-term, band-aid fixes, eventually leading to long-term health issues.

5. Sleep
“At night I used to wake up and sit up, wondering what I’m going to do.” — A caregiver whose father-in-law had a life-altering accident
For almost all the caregivers we spoke to, disrupted sleep, sleepless nights, and the possibility of having to wake up in the middle of the night to attend to the needs of the patient were a part of their everyday reality. This eventually affected their mental and physical health, with many caregivers reporting that they were unable to concentrate on their studies or work.
6. Work and education
“For two months after she passed, I couldn’t concentrate on work. It was very emotional for me. I lost my job eventually.” — A caregiver whose late grandmother had liver cirrhosis
For most caregivers, regular, stable routines were almost non-existent. They had to sometimes rush home from work during emergencies, take time off for caregiving duties, and occasionally defer important appointments and exams. Ultimately, this had a detrimental effect on their professional growth as well as acted as a barrier to opportunities they may have otherwise been able to pursue, putting them in an emotionally vulnerable position and adding to their distress.
7. Personal time
“We can go out as a family about once a month, only if we’re able to get someone to watch her. As parents, we have to take our son out to places like the park too, right? — A caregiver whose mother-in-law had a stroke
Before becoming a caregiver, people had the time to socialize with friends, watch movies, and relax. As caregivers, however, there were limited opportunities to spend quality time with family and friends due to multiple caregiving responsibilities. This, in turn, affected their own sense of mental wellbeing, spawning feelings of regret and guilt of not spending time with their children.
8. Finances
“We have already taken so many loans, how much more can we take? Now we can’t take him to the hospital anymore.” — A caregiver whose husband had hypertension and experienced a stroke
Prior to becoming caregivers, people relied on their salaries or daily-wage incomes to meet expenses. With growing healthcare expenses, many had to take loans that went beyond their income. Others sold land and/or sought out financial support from close relatives. Typically, this leads to high debt levels for many years of their lives, high stress levels in finding the means to pay them back, thus affecting the livelihood of the family.
Many times, the increasing financial burden also caused patients to drop off from the health system and treatment plan due to its unaffordability. In some cases, children were pushed into jobs after getting a basic education or made to help out in the house, eventually hindering prospects of a better future for them and their families.
9. Transport and logistics
“It’s difficult to take him to the hospital in the bus, so we had to take him in a car. Transport and hospital expenses used to be INR 3,000 – 5,000 per day” – A caregiver whose son had epilepsy
Before becoming a caregiver, transportation involved walking, using public transport, or a two-wheeler vehicle. With patients, due to their inability or the fear of infection, these modes became difficult to use. And so, caregivers had to organize a car, ambulance, or auto rickshaw if they wanted to take the patient anywhere — especially to hospitals that are far away. All of these are significantly more expensive, added to the existing severe financial strain, and increased the family’s dependency on others.
Visualizing the caregiving load
The caregiving burden (or strain) is a multidimensional concept that reflects how caregiving adversely impacts their emotional, social, financial, physical, and spiritual functioning. From our research it became even more evident that becoming a caregiver came with substantial life changes.
However, translating the richness of our findings proved challenging. When it comes to qualitative insights, graphs and maps only convey so much, obscuring many of the human subtleties and nuances. And so, we set out to understand alternative ways to best communicate the wealth of data from our observations and interviews without losing the complexity and emotions that were shared by each caregiver.
Ultimately, we landed on two different approaches to communicate the bittersweet nature of a caregiver’s journey:
- Storytelling: We compiled a set of three caregiver stories, drawing on the real conversations we’d had during our research, but dramatized to facilitate fictional writing. The use of fictional writing allowed us to bring to light the complex thoughts and feelings experienced by caregivers and help the reader engage with the research better to really understand the points where caregivers could use more support. It also contains a visual map depicting these challenges and how they navigate various parts of the health system ineffectively, due to a lack of information.
- Data visualization: We presented the data in an easily digestible format, while also stirring emotion. To do this we decided to leverage data humanism — a form of presenting data that involves linking numbers to relatable concepts and behaviors that encompass the subjective and imperfect aspects of human experience. Simply put, data humanism blends quantitative analysis with a focus on uncovering the human narratives embedded within the data.
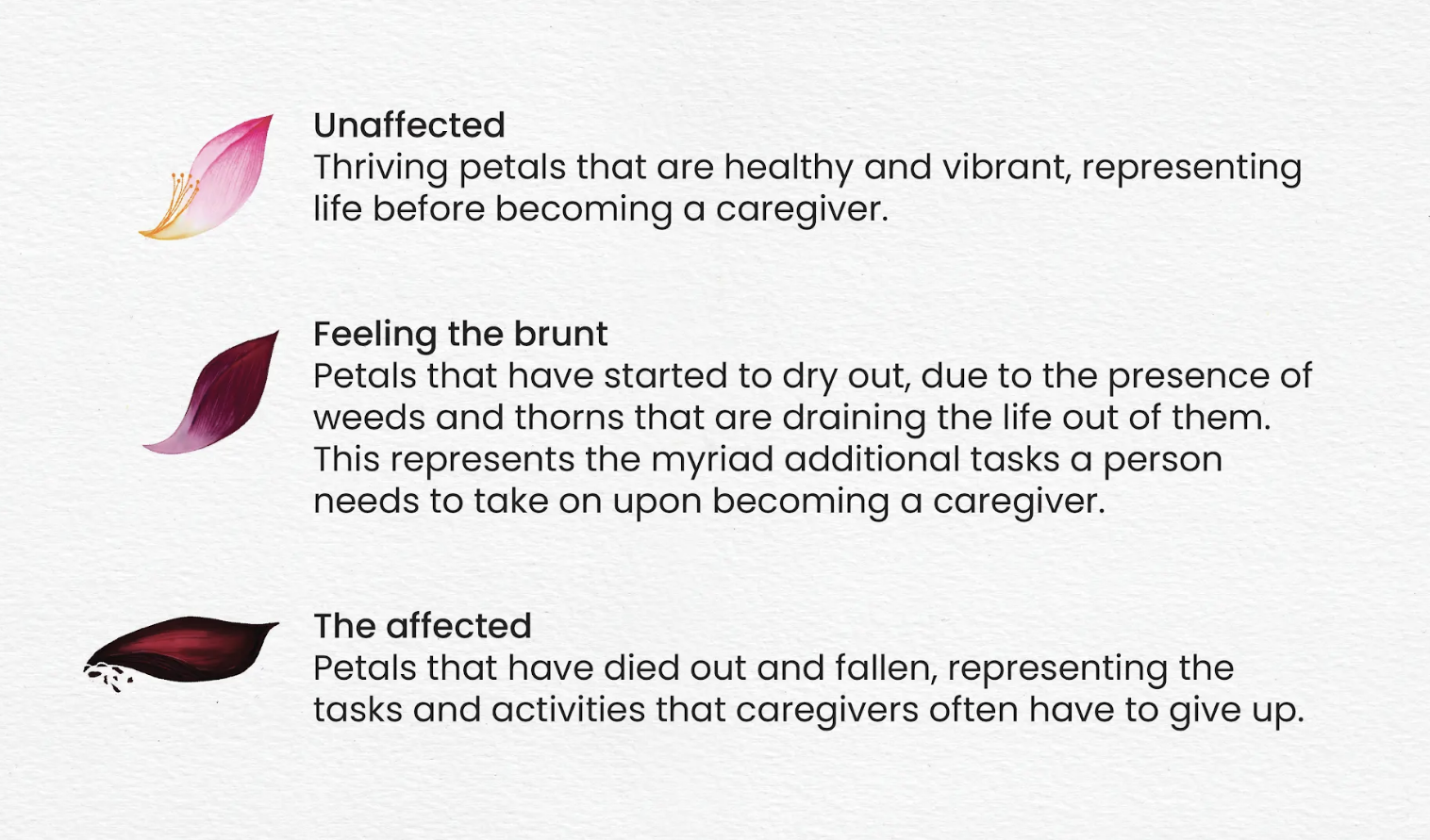
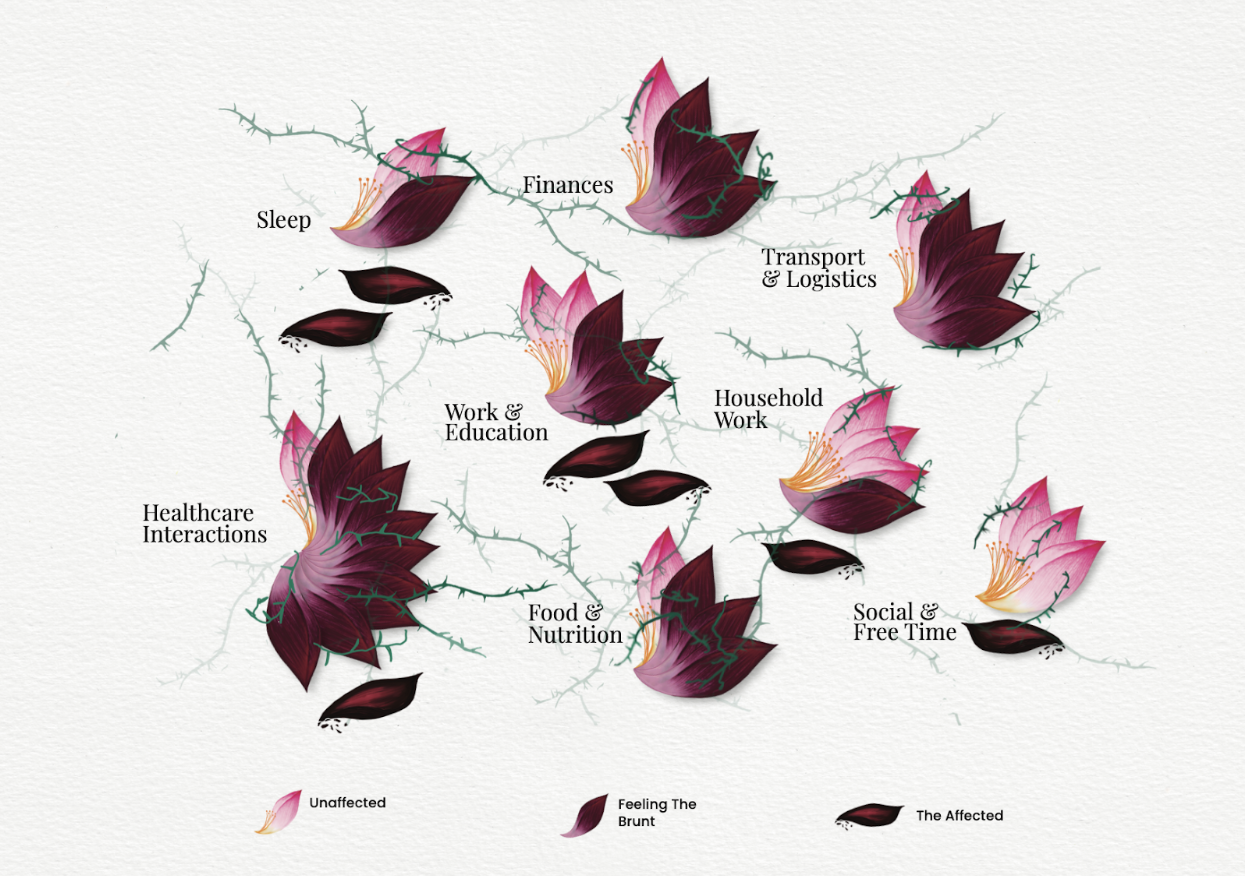
The way data humanist Giorgia Lupi used natural elements in her work titled Bruises — The data we don’t see, inspired us to do something similar in our visualization. In our various explorations, we saw parallels between the load of caregiving tasks affecting caregivers and the impact weeds and thorns have on flourishing flower petals. After several rounds of sketching and feedback, we narrowed in on a visualization with three distinct units, each conveying a unique aspect of our findings.
The resulting visualization, titled The Caregiver’s Load, illustrates how the responsibilities that a caregiver takes on are neither easy nor minor. This role is life-altering and often entails a long and difficult journey with many obstacles. One can never be fully prepared for it. While caregiving has its gratifying and warm moments, the emotional stress it brings makes it difficult to sustain this role long-term.
From data to action
Through this project, our goal was to both deepen our understanding of caregiving and to spark conversations about how we can further support caregivers through our work. Both the data visualization and caregiver stories were shared at multiple conferences and events. The overwhelming feedback we received was that the analogy to a flower petal allowed people to relate to the load a caregiver carries, at a much deeper level.
One of the key takeaways from our research was that there’s a substantial gap in the availability of emotional support for caregivers.
Not only does this take a toll on a caregiver’s physical and mental well-being, it also limits their ability to support ill family members, eventually affecting patient outcomes.
To address this issue, in the next phase of the project, we explored what effective emotional support might look like for these caregivers, and co-designed interventions with them to understand what is practical and sustainable long-term.
Our findings are built into The Care Toolkit — a comprehensive resource that can act as inspiration and a practical guide for people and organizations looking to create emotional support interventions for caregivers. We’ll be sharing this publicly soon, so keep an eye out for it!
From a gender equality perspective, our research also showed that there is a pressing need to share the physical and mental load of caregiving among different family members — both male and female — by increasing awareness about ways they can contribute and be more involved. However, this is a broader issue that stems from existing gender stereotypes, creating a need for special care and support for women carrying out caregiving responsibilities.
To ease the burden for family caregivers and to allow them to sustainably continue doing what they do, we need to build products, services, and policies that center their needs. Our insights are a tiny glimpse into caregivers’ complex lived realities, and we hope to continue to build on them alongside other individuals and organizations striving to make caregivers’ lives just a little bit easier.




